Just pronounced one of my favourite patients to date. She managed to stay until she had her Christmas Eve party in her home.
Happy and sad tears.
And something so beautiful about saying goodbye to my own patients in the way they want.
Wednesday, December 24, 2014
Thursday, December 18, 2014
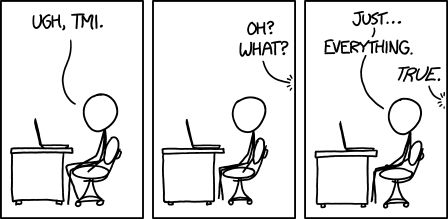
Too much
A few weeks ago, my class song started playing. Usually I don't just sing along, I bang my head and call all my med school friends.
This time though, I did nothing. But I did realise that I was in trouble. It became clear that what was going on in my professional life was affecting my personal life.
This is what burnout looks like to me.
Saturday, November 8, 2014
Who is having the heart attack here??
Ran a code STEMI a while ago. We are more than 1 hour from PCI so we do all the clot busters in our wee hospitals cross our fingers and go to the nearest cath lab.
Obviously there is a long discussion about the pros and cons of using the busters. There are risks of bleeding. Our patient's medical history is reviewed to rule out any chance of bleeding.
As we piled into the ambulance my patient's wife started crying. She said that she was remembering when her husband had hiis AAA burst and how scary that had been.
o.0
It took me a minute to realise that she meant her former husband.
Thursday, November 6, 2014
Women physicians are smart enough to kill themselves but not as clever at finding help
"A widely cited decade-old meta-analysis suggests that the suicide rate among male physicians is 40% higher than among men in general, while the rate among female physicians is 130% higher than women in general (Schernhammer ES and Colditz GA. Am J Psychiatry. 2004;161[12]:2295-2302)."
Monday, November 3, 2014
Happiness is...
Shaking the hand of the patient you ran a code on 2 weeks earlier when they've been repatriated to your wee hospital.
Sunday, November 2, 2014
Fighting with my sense of self...
I keep hearing "advice" from folks:
1. Fire the difficult patients.
But who will take care of them? They're the ones that are always being left. How could I possibly be another one in a long line of people who abandon them?
2. Be more like Doc Marten. (If you haven't seen the TV series on Netflix yet, check it out.)
Doc Marten is a fantastic diagnostician but is an absolute ass. Patients don't want to be around him. He treats his staff, his patients, and his colleagues like they are subhuman. No. Just no.
3. Ask for help.
I have been asking for help for a year now. Occasionally these requests are masked as jokes. More often they are unofficial sit downs. I've asked colleagues, office managers, staff, nurses and therapists. Unfortunately, the culture of medicine dictate that docs don't need help. Ever. So I needed to make an ass of myself to be heard.
4. It gets better in 5 years.
Really. Brilliant. And until then, how do I keep myself from imploding? It's true that having a light at the end of the tunnel is helpful. However, as anyone who has ever been overwhelmed with anxiety knows, the future is something that happens to other people.
5. Don't get involved in your patients' lives and anything but their immediate health.
No. Just no. I refuse to pretend that my patients aren't people to make it easier when they die, make it easier to ignore their mental health problems and chronic pain. When I stop crying with and for my patients, it's time for me to quit.
Friday, October 31, 2014
Friday, October 24, 2014
My moral fortitude is taking a beating
I keep thinking that it will get all better but I'm worried I'm wrong.
I think every patient deserves to be treated with respect and that each of their concerns deserve consideration. They don't necessarily need to be dealt with immediately but at least a passing thought must be paid to them.
I feel like to make this happen in my current working condition I need helpers. I feel like I'm being encouraged to not treat patients well and to write off certain conditions like depression and anorexia as lost causes. That I'm wasting my time for helping my patients with obesity stay motivated.
The grumbly, crusty outlook that so many of my colleagues have developed over their years of practice is expected to take over me all at once now that I'm practicing.
I feel like I'm having a true crisis of faith.
Wednesday, October 22, 2014
Check those out!
We have ads in our offices of see through people that are promoting colon cancer screening.
A patient and I were chatting today about how much easier my job would be if all my patients we're see through.
Monday, October 20, 2014
Patients say the funniest things
Patient one: I was wondering if I can have some sleeping pills for my inzombia.
Me: pardon? Your what?
Pt 1: inzombia
Me: bahahhahaha - oh.
Patient two, after sending her to do a swab in the washroom, calls me from the washroom: how do I put the swab into the tube?
Me: take the lid off?
Pt 2: how do I? Oh. Ok. Got it.
Tuesday, October 14, 2014
That moment...
That moment during a code when you realise this is only the second one you've run but things seem to be going smoothly. Don't jinx it!
Pabst Blue Ribbon
Definitely wrote a note to the surgical team at Teriary Care Centre with the following:
Patient was transfused with 3 units PBR.
Rather than the 3 units PRBC (packed red blood cells) he actually got.
Monday, October 13, 2014
Buggy
I am now on my third virus in two weeks. I hope that at some point I grow an immune system. Otherwise I may never make it to my fifth year of practice when everything is supposed to come together.
Friday, October 10, 2014
Dating naked
Pt who is up all night: so there's this show on at 2 am called Dating Naked and I watch it while I do laundry. Not for them obviously.
Monday, October 6, 2014
Pro Tip
If the night nurses are willing to do a terminal clean on a room (i.e. scrub all surfaces including the floor) so you can admit a Form 1 from the office, you bet your booty you're buying them all ice cream and frozen yogurt.
Ice cream and frozen yogurt is always a winner.
Thursday, October 2, 2014
Tuesday, September 30, 2014
Perspective
Got to see a couple of my favourite kids in my practice. They're loud and busy and not at all shy.
Thing 2 was sitting at the end of my exam table on my wheely stool. He pulled out the stirrups and told us these were obviously for his elbows. Obviously. He then proceeded to go through the drawers and pull out speculums, pads, swabs, pap brooms, etc. and "mix a potion".
So silly. So awesome.
After getting his vaccine, he stomped off down the hall to find my candy stash and grab an extra handful.
I wasn't invited
Sweet old man with known prostate cancer, as I try to explain that he now has mets to his spine. "So the cancer moved out of my prostate and into my spine?"
"No. Your prostate cancer had babies and sent them to your spine. "
"Oh. They didn't even invite me to the baby shower!"
"Well, cancer is a jerk."
Wednesday, September 24, 2014
Terrifying noise
Just getting to sleep, window open, when I hear an ambulance at full tilt and a helicopter. I'm off call entirely, but because I'm in town it's reasonable to ask me to show up if they need more hands.
The questions going through my head:
- am I going to get called in?
- is it one of my patients?
- is it one of my neighbours?
- did I miss something the last time I was in the Emerg?
- would I have been able to handle whatever is going on in the Emerg tonight?
So much for sleeping tonight.
Saturday, September 6, 2014
Zestfully pronounced
TV show: image of police officer checking pulse of clearly frozen guy on the side of road, calls in a death for a coroner
Me: well, you know what they say about being cold and dead....
My partner: that it's better to be cold than dead?
Me: no....
My partner: that's what they should say
Me: they say that someone isn't dead until they're warm and dead
My partner: that sounds like "you're not fully clean unless you're zestfully clean"
Me: exactly, only based on real science
Wednesday, September 3, 2014
Professionalism
Especially at this time of year, when med students are being introduced to their profession, I hear the word professionalism getting thrown around. It drives me a little crazy because what the administration, vice deans, etc. actually mean is "please don't embarrass us".
The subtle threats of discipline are based on a very narrow definition of professionalism. The powers that be (PTBs), want med students to behave like sweet children at all times. Med students should drink responsibly. They should use Facebook for only chaste reasons. They should not introduce themselves as doctor until they have actually finished med school and have an MD.
The PTBs are a little right. These acts are indeed part of what makes a medical student professional. But to become physician whose colleagues will consider professional, there are many more "soft" skills these students need to become proficient with.
1. Social Media. SoMe is not the devil. It should be embraced by physicians and those in training. This article does a good job of briefly outlining the risks and benefits of practicing medicine in a world with social media. I use Twitter to keep on top of new research in family medicine and emergency medicine. Following FOAM articles on Twitter and blogs puts the basics learned in classrooms into a clinical perspective so that students' medical education is integrated, and, more importantly, self directed.
2. Self directed learning. To continue growing as a physician, we need to keep ourselves motivated to follow clinical questions that pop up during the day, and learn the skills required to do this. The idea of a flipped classroom starts to put the onus on students to prepare and do work outside of the classroom. I dream of a med school where all the teachers are passionate about their subjects and happy to put effort into preparing both the pre-work and the actual activities. Can you imagine these teachers working together to bring med students from being given predigested information to being able to answer questions similar to what will come up in real life practice? Encouraging students to feel comfortable asking for clarification? Moulding these students into future colleagues they want to work with?
Ideally by the end of the classroom portion of med school, the students would be ready for self evaluations of their work. Students should feel comfortable with what they do and do not know, and being comfortable with the vulnerability needed to ask for their teachers' opinions of their progress.
3. Communication. Not just using your doctor words, but learning how to have conversations with colleagues that are uncomfortable. Being able to disagree, admit you were wrong or that you made a mistake, asking for help, asking someone who knows more about a topic to teach you. These are all skills a professional doctor possesses. Our small groups, flipped classrooms, and clinical teaching environments are perfect places to cultivate these skills. We should be encouraging all teachers to work on communication with their med students while also teaching how to take a pulse. Praise the student who says they have no idea what they are supposed to be feeling for in a pelvic exam or are not sure how to read the chest x-ray. Don't demean these students or treat them like they're a waste of your time. These are the future colleagues that won't be too cocky to ask for the second opinion that could save a patient's life.
4. Self Care. A burned out physician is useless to their patients and to their colleagues. Learning how to take care of their mental and physical well being needs to get more than just lip service in medical schools. I have a lot more to rant about this, and will. Later.
5. Advocacy. Pick something that you love. Learn more about it. Make the world a better place. Most PTBs are pretty good about encouraging this, especially because when med students do good things, it makes up for all those times they embarrass their schools.
6. Compassion for each other. The competition that got us into med school can turn into icky feelings when we are thrown together for more than 4 years of intense, sleep deprived, time together. It's time to learn how to get along, how to make each other into the best docs possible. This includes all that I mention above. Do you have a secret that makes studying for anatomy a lot easier? Share it with your anatomy table, or hell, why not the whole class. Is someone missing from class for days at a time? Quietly check in to see if they need notes, a beer, or a shoulder to cry on. Something my small groups and I do is a weekly "check in" to encourage this behaviour. We start our sessions by discussing what important (or interesting) thing happened this week. I learned about my students' struggles with head and neck anatomy and watched as they helped each other through it. When a student disclosed a horrific event from his past, I was proud to see his classmates reaching out figuratively and literally to console him and thank him for sharing.
Medical students want to make the world a better place. Practicing professionalism through their education will help them to make that happen.
The subtle threats of discipline are based on a very narrow definition of professionalism. The powers that be (PTBs), want med students to behave like sweet children at all times. Med students should drink responsibly. They should use Facebook for only chaste reasons. They should not introduce themselves as doctor until they have actually finished med school and have an MD.
The PTBs are a little right. These acts are indeed part of what makes a medical student professional. But to become physician whose colleagues will consider professional, there are many more "soft" skills these students need to become proficient with.
1. Social Media. SoMe is not the devil. It should be embraced by physicians and those in training. This article does a good job of briefly outlining the risks and benefits of practicing medicine in a world with social media. I use Twitter to keep on top of new research in family medicine and emergency medicine. Following FOAM articles on Twitter and blogs puts the basics learned in classrooms into a clinical perspective so that students' medical education is integrated, and, more importantly, self directed.
2. Self directed learning. To continue growing as a physician, we need to keep ourselves motivated to follow clinical questions that pop up during the day, and learn the skills required to do this. The idea of a flipped classroom starts to put the onus on students to prepare and do work outside of the classroom. I dream of a med school where all the teachers are passionate about their subjects and happy to put effort into preparing both the pre-work and the actual activities. Can you imagine these teachers working together to bring med students from being given predigested information to being able to answer questions similar to what will come up in real life practice? Encouraging students to feel comfortable asking for clarification? Moulding these students into future colleagues they want to work with?
Ideally by the end of the classroom portion of med school, the students would be ready for self evaluations of their work. Students should feel comfortable with what they do and do not know, and being comfortable with the vulnerability needed to ask for their teachers' opinions of their progress.
3. Communication. Not just using your doctor words, but learning how to have conversations with colleagues that are uncomfortable. Being able to disagree, admit you were wrong or that you made a mistake, asking for help, asking someone who knows more about a topic to teach you. These are all skills a professional doctor possesses. Our small groups, flipped classrooms, and clinical teaching environments are perfect places to cultivate these skills. We should be encouraging all teachers to work on communication with their med students while also teaching how to take a pulse. Praise the student who says they have no idea what they are supposed to be feeling for in a pelvic exam or are not sure how to read the chest x-ray. Don't demean these students or treat them like they're a waste of your time. These are the future colleagues that won't be too cocky to ask for the second opinion that could save a patient's life.
4. Self Care. A burned out physician is useless to their patients and to their colleagues. Learning how to take care of their mental and physical well being needs to get more than just lip service in medical schools. I have a lot more to rant about this, and will. Later.
5. Advocacy. Pick something that you love. Learn more about it. Make the world a better place. Most PTBs are pretty good about encouraging this, especially because when med students do good things, it makes up for all those times they embarrass their schools.
6. Compassion for each other. The competition that got us into med school can turn into icky feelings when we are thrown together for more than 4 years of intense, sleep deprived, time together. It's time to learn how to get along, how to make each other into the best docs possible. This includes all that I mention above. Do you have a secret that makes studying for anatomy a lot easier? Share it with your anatomy table, or hell, why not the whole class. Is someone missing from class for days at a time? Quietly check in to see if they need notes, a beer, or a shoulder to cry on. Something my small groups and I do is a weekly "check in" to encourage this behaviour. We start our sessions by discussing what important (or interesting) thing happened this week. I learned about my students' struggles with head and neck anatomy and watched as they helped each other through it. When a student disclosed a horrific event from his past, I was proud to see his classmates reaching out figuratively and literally to console him and thank him for sharing.
Medical students want to make the world a better place. Practicing professionalism through their education will help them to make that happen.
Tuesday, August 5, 2014
Goat women
Sunday, August 3, 2014
Shame, vulnerability and the Impostor Syndrome
Take a look at this TED talk.
Brené did a mixed methods study on connection and shame and unexpectedly found that at the base of our connections was our comfort with vulnerability.
“Connection is why we’re here. It gives purpose and meaning to our lives”. Connections are the basis for all social interactions. It is impossible as a physician to ignore connections in our daily lives. I think of the usual connections when I say this, the relationships we have with our patients and their families, our colleagues, our community, our own families and friends, and ourselves. Brené suggests that shame unravels connection. Shame makes us feel unworthy of connection. Underpinning the shame was excruciating (not comfortable) vulnerability. Impostor syndrome strikes again!! I’m not smart, thin, fit, happy, well enough to be a doctor. The sense so many of us feel that there was a mistake including us in the Hippocratic Oath.
In this study Brené describes a subset of her population as having a sense of worthiness, a strong sense of love and belonging, and who also believe they are worthy of love and belonging. Brené calls these “whole hearted” people. She found they had a sense of courage, originally defined as telling the story of who you are with your whole heart. They had the courage to be imperfect. They had the compassion to treat themselves well first, then someone else, because we can’t be kind to others unless we are kind to ourselves. Lastly, they had connections in their lives because they were brave enough to let go of who they are. They fully embraced vulnerability, believing that what made them vulnerable made them beautiful, a necessary (if occasionally difficult) willingness to invest themselves in something that might not work out. To me, all docs must at some level be these whole hearted type folks. To apply for medical school, to write the MCAT, to apply for residency and finally join a practice requires an acceptance of our vulnerability, even if we, like everyone else we struggle with it.
“We numb vulnerability” with substances, poor behaviour, food, work, etc., but Brené suggests that this numbs all of our emotions as well. Essentially, if we are unable to allow ourselves to feel vulnerable, that we won’t feel joy, sadness, etc. There are lots of reasons for docs to feel vulnerable as we constantly flirt with the unknown, perform tasks others wouldn’t dare, etc. We also know lots of ways to feel numb.
Certainty for us comes in the form of, well, forms and checklists and Evidence Based Medicine. If we can point to a study that allows us to stop/start/increase/decrease a statin, we can make a choice that we don’t have to worry about. I’m not advocating for a return to paternalistic medicine, but that we continue to treat the patient, not the numbers. Even writing that makes me feel uncomfortable. What if my patient has a stroke that is debilitating and decides to sue me because I didn’t push hard enough to keep her on a statin? Making choices with our patients in a patient centred way requires us to feel vulnerable in several ways. We are allowing our patients to know that we don’t know all the answers. This flies in the face of many of my preceptors who advocated that I pretend I know what I’m doing and talk about my proposed treatment plan as though it was unquestionable to make the patient feel comfortable. As I’ve talked about before, there are thousands of new journal articles published every week making it impossible for us to keep up on everything, especially if we are generalists. I think it takes courage to prescribe ANYTHING given that there may be a time in a few weeks or a few years that this med is considered as useless as blood letting (or is that back in fashion again). Nutritional advice is a perfect example of how information flip flops. Again though, we are encouraged in our training to stand by our published guidelines of our various groups. These are helpful to be sure, but are still just guides to helping patients make decisions.
Being taught explicitly and implicitly through paternalistic modelling, I rarely had a chance to feel comfortable in my uncertainty as a learner. Thinking about answers when I was being pimped, trying to consider more than one organ system in treatment plans, offering more than one treatment for an illness was discouraged. I was to be confident at all times, and if I didn’t feel it, I was to fake it. I was punished with poor grades if I acknowledged uncertainty in my assessments and plans. It makes allowing myself to feel vulnerable in my practice difficult.
One step I’ve taken to correct this is to find my own therapist, and as Brené suggested, I found one who is a therapist for therapists - “it’s necessary because their bullshit meter is higher”. You know it’s true. Anyone who has ever done time in the ER with psych patients knows how to say what needs to be said to ‘pass’ your suicidal ideation screen. She is not a therapist of other doctors though which has provided me with a refreshing insight into what I’ve learned to take as gospel. She will frequently say, what? does everyone think that is reasonable?? and help me to find my place in this community.
We need to believe that we are enough. This rewards our courage to feel vulnerable in front of our patients and colleagues and sets the stage for an ability to feel grateful and well in the future. It sounds that uncertainty and vulnerability is something we can practice until we are comfortable with. We should promote vulnerability in our learners. We need to talk about the shaming that occurs in our profession (these young docs, thinking they should only take on 1000 patients at a time; oh, vacation AGAIN?, etc.) and show its ridiculous nature. Shame has no place in a doctor’s professional and personal life if at the end of our day we have completed our job to the best of our abilities. It doesn’t need to be perfect or neat, but given the resources of the day, it will be enough. The connections we have with other people in our lives will be stronger, and, hopefully, quiet the shaming and impostor syndrome voices.
Saturday, August 2, 2014
I speak fluent poverty
It doesn't make me terribly popular with administration folks. I've recently been accused of being unprofessional. This stems from the way I talk about and to patients.
I treat my patients as thinking, feeling beings who can make their own choices about their health and their life in general. I call them out on their bullshit and try to find out why they're making the choices they do. There's no point in preaching at a patient about not eating fruits and veg if the food bank has been out for a month.
I don't use flowery language because unfortunately, most of my patients are illiterate. When I started practice, I assumed many would be health illiterate, but I certainly wasn't expecting this. My staff has stepped up (I love them so) and help my patients to fill out the millions of forms that we process every month. I've stopped playing along with "I left my glasses at home" and ask them straight out how their reading is. They've been so used to lying about it, it takes them back and puts them on the defensive for a minute or two until they realize there's no judgement, just me looking to do best by them. I've gotten into the practice of reading out my referral letters to my patients so that 1. I have to finish it while I'm in the room with them, 2. they know what I'm saying about them and 3. they can correct me as I go along. My patients frequently laugh at my "doctor words" that go into those letters. That lets me know that the way I'm speaking with them is different than how I speak with other docs. I like that.
From the stories I hear from my patients, they haven't had someone who will actually listen in a long time. They get painted with the same brush as their drug dealing brother, as their morbidly obese mother, and as their father who has been in and out of jail since they were born. These folks are rarely treated as an important individual.
The same approach works for those patients I have with money and more stable upbringing. I fancy up my language, but otherwise, I continue to treat them as individuals. I don't care that you were mayor for 20 years, we are just starting a relationship, I want to know WHO you are, not what other people see you as.
Part of my approach has to do with my appearance. I've written about this before and I think I've made it clear that I am an untraditional appearing doctor. Most patients ask to see the doctor after I've been in, even when I clearly introduced myself at the beginning. Their response is not one of disbelief but of relief. "oh! you're like a real person!". I'm a bit quirky, I'm overweight, I smile all the time, especially when I don't feel like it. When my patients die, or I need to give someone bad news, or someone has divulged some horrific part of their life, I cry with my patients. It's the only way I can think of to let them know that they matter to me.
I also have a strong feeling for what is and is not fair. This is something that comes through whenever I talk to a child living well below the poverty line. Their anger and emotional outbursts are almost always associated with a feeling that something that has happened is unjust. I grew up well below the poverty line and I still get surges of rage when things are unfair. I've learned to breath deeply, reconsider my stance, and decide whether or not I need to proceed. If I need to proceed, look out. It will feel like molten lava is being rained on your head, because on top of my previous poverty speak, I am now also fluent in affluence, biz speak, economics, and ethics.
This all sounds very Polly-Anna-y, and it might be. Putting my personality in with a hospital that has administration that could, easily, use walkers, doesn't always work. I'm optimistic though that I can persuade admin to my side even through continuing to be patient centred. It's in the mission statement of every hospital of Ontario, including ours.
I don't use flowery language because unfortunately, most of my patients are illiterate. When I started practice, I assumed many would be health illiterate, but I certainly wasn't expecting this. My staff has stepped up (I love them so) and help my patients to fill out the millions of forms that we process every month. I've stopped playing along with "I left my glasses at home" and ask them straight out how their reading is. They've been so used to lying about it, it takes them back and puts them on the defensive for a minute or two until they realize there's no judgement, just me looking to do best by them. I've gotten into the practice of reading out my referral letters to my patients so that 1. I have to finish it while I'm in the room with them, 2. they know what I'm saying about them and 3. they can correct me as I go along. My patients frequently laugh at my "doctor words" that go into those letters. That lets me know that the way I'm speaking with them is different than how I speak with other docs. I like that.
From the stories I hear from my patients, they haven't had someone who will actually listen in a long time. They get painted with the same brush as their drug dealing brother, as their morbidly obese mother, and as their father who has been in and out of jail since they were born. These folks are rarely treated as an important individual.
The same approach works for those patients I have with money and more stable upbringing. I fancy up my language, but otherwise, I continue to treat them as individuals. I don't care that you were mayor for 20 years, we are just starting a relationship, I want to know WHO you are, not what other people see you as.
Part of my approach has to do with my appearance. I've written about this before and I think I've made it clear that I am an untraditional appearing doctor. Most patients ask to see the doctor after I've been in, even when I clearly introduced myself at the beginning. Their response is not one of disbelief but of relief. "oh! you're like a real person!". I'm a bit quirky, I'm overweight, I smile all the time, especially when I don't feel like it. When my patients die, or I need to give someone bad news, or someone has divulged some horrific part of their life, I cry with my patients. It's the only way I can think of to let them know that they matter to me.
I also have a strong feeling for what is and is not fair. This is something that comes through whenever I talk to a child living well below the poverty line. Their anger and emotional outbursts are almost always associated with a feeling that something that has happened is unjust. I grew up well below the poverty line and I still get surges of rage when things are unfair. I've learned to breath deeply, reconsider my stance, and decide whether or not I need to proceed. If I need to proceed, look out. It will feel like molten lava is being rained on your head, because on top of my previous poverty speak, I am now also fluent in affluence, biz speak, economics, and ethics.
This all sounds very Polly-Anna-y, and it might be. Putting my personality in with a hospital that has administration that could, easily, use walkers, doesn't always work. I'm optimistic though that I can persuade admin to my side even through continuing to be patient centred. It's in the mission statement of every hospital of Ontario, including ours.
Thursday, July 31, 2014
Disappointment
A couple in my practice was very upset with me. They felt that I hadn't responded quickly enough to their requests for information. They're right, I didn't. Nothing bad happened. Everything turned out well. But still.
It shook me.
I am supposed to be perfection incarnate. I should be everything to everyone of my patients and make them feel safe. I shouldn't add stress to their already stressful times.
At the point in question, I had taken one week vacation 5 months earlier and likely had 5 days off in those 5 months. I was working late most days and working every weekend. I was tired and I was starting to not care.
I recognized this and scrambled to get a locum and took off for 2 weeks. It barely scratched the surface of my exhaustion but helped me gain a little perspective and the distance needed to come up with a plan to keep things on track.
I'm still not perfectly on track, especially when I'm having bits of my soul torn out by patients instead of making their specialist referrals, but I'm making progress.
The plan to not slip further behind was fairly simple. I don't leave a patient encounter without completing all paper work associated with that encounter.
It means I'm running 15 min behind on most days and typing madly as I sit with the patient. I'm also messaging staff to bring me pages I need from the outer office. On most days, I can feel confident I've done enough to continue treading water. I'm not getting any further ahead, but mostly I'm not sinking. Not much any way.
I know in my head that it's not reasonable to think I'm not allowed to make mistakes, but it doesn't seem to make it to my heart. Could that be something I might have been able to learn prior to jumping in to my practice? Is it something I'll ever be comfortable with? I'll certainly continue working on being kind to myself. It's a never ending battle.
Saturday, July 5, 2014
Kill the demons
I keep trying to find ways to chill out in the shortest amount of time possible. My days tend to be filled with emotionally and physically exhausting hours making it necessary for me to recharge.
I've been playing a lot of Diablo 3.
There's something very satisfying about clearing a level of all its demons. Maybe it feeds my OCD tendencies to scour every inch of the terrain for loot, gold, and monsters to kill.
I'm able to complete quests in less than a day. In real life, my quests for answers to patients' ailments can take weeks and longer. And, even then, instead of a huge pile of gold and super swag to dress my hero, I just have a patient with a shiny new cancer.
Knowing the demon I'm now fighting with my patient helps both me and my patient (the devil you know?). Instead of minions, I fight paper work. Instead of shamen, my patient fights nausea. Rather than gold and swag, we get kudos and some days of feeling well.
Looking at my work pile as a quest helps. Seeing my nurses, secretaries, PT, OT, and the rest of the team as my guild, each with their own skills to reach our goals also helps.
But still not as satisfying as sitting and killing hundreds if demons in one sitting.
Tuesday, June 17, 2014
Sunday, June 8, 2014
Tuesday, June 3, 2014
Working it
Patient re breast prosthesis: that's my working boob
Me: (imagining granny in hooker shoes on the corner of main)
Patient: you know, for sweating in and doing housework
Me: Bwah hahahahha
Tuesday, May 27, 2014
Sunday, May 25, 2014
Information Overload
There is just way too much to assimilate in an orderly fashion. Everything from the marital status of my patients, hip clicking syndrome is a thing, billing codes, anything new in the literature.....
XKCD
No great words of wisdom, no tricks I've found for dealing with this (aside from putting everything patient related into the EMR, no matter how trivial, and everything knowledge related into Evernote with extensive labels).
I keep being told that I will know my patients in 5 years and that things will seem better then. The patients that I am getting to know do make my days easier to deal with. Instead of having to look up their comorbidities constantly, I have a handle on what may be causing the crisis du jour. That very few of these illnesses are actually controlled yet is a whole other issue.
Friday, May 9, 2014
I may have been this doc
(608): The only thing worse than cracking my rib on a slip and slide was having the doctors laugh when they found out in my medical history that I did this exact same thing last summer.
TFLN
Monday, April 28, 2014
Sunday, April 13, 2014
Hunters
Many of my new patients are hunters. They bring their game home, butcher and eat, freeze or dry it.
I would never do it. It's not my thing at all, but I get why hunters like it. It's not just a sport, it's how they ensure antibiotic free meats for their families.
But it makes me wonder, are hunters just lazy farmers?
Thursday, March 13, 2014
That moment when
I finally find out I'm not the only new doc who feels in over their head and like I've made the biggest mistake ever.
And as a result finds wine extra tasty.
Tuesday, March 11, 2014
OMG
There's money in my bank account. It's been there for more than a month. It's ridiculously confusing. And delightful.
Sunday, March 9, 2014
That moment when
The drunk guy's face looks better after you've finished suturing it up than it did before he, um, walked into the middle of a fight.
Friday, March 7, 2014
That moment when
I choose a bowl of cereal over a Blue Menu microwave meal because the microwave dinner takes too much effort.
Wednesday, March 5, 2014
The root of my discomfort
I've been pretty uncomfortable with my practice for a few months. I keep being told it's normal and it will get better in a few years, but I'm seriously having a hard time getting to work some days.
After talking it out with my VERY patient partner, I think that my unease comes from more patients than time. He asked what would make life better for me right now. Some things are fairly easy like a housekeeper to deal with my dirty socks and ring around the tub.
But the big answer was a month off with a locum covering my practice so I could make care plans for my patients. Some of them have diseases I've never heard of. How can I possibly feel comfortable treating them??
I guess that's where the extra years in practice comes in?
Friday, February 21, 2014
Anger
So many of my new patients are so, so very angry at their previous docs. I expected some disgruntled patients, but many of my new patients are incredibly upset.
Most of them feel like no one has been listening to them. I'm not doing much different from the previous docs, and truly feel like I'm rushing them out of my exam rooms. I worry like crazy that I'm going to eventually become a doc who they think is not listening. It may be that their docs were listening but because I'm a fresh face, now they feel heard.
They also are angry that diagnoses are missed. For me, it's been easy. I see all the symptoms in chronological order. I see what's been ordered and what's left. I see what's been ruled out. It makes me look like a genius when it just means I've done my homework.
Then there's the racist, genderist, homophobic etc. comments that I get as well. I try to stop my patients from talking before they say something I'LL regret because it means that I'll hear it again whenever I see their face.
No great lesson from all this. Just legitimate worry for my future and trying to figure out why it's like this.
Subscribe to:
Posts (Atom)